- Research article
- Open access
- Published:
Cardiovascular disease (CVD): assessment, prediction and policy implications
BMC Public Health volume 21, Article number: 1299 (2021)
Abstract
Background
The study aims to predict and assess cardiovascular disease (CVD) patterns in highly affected countries such as Pakistan, India, China, Kenya, the USA, and Sweden. The data for CVD deaths was gathered from 2005 to 2019.
Methods
We utilized non-homogenous discrete grey model (NDGM) to predict growth of cardiovascular deaths in selected countries. We take this process a step further by utilizing novel Synthetic Relative Growth Rate (RGR) and Synthetic Doubling Time (Dt) model to assess how many years it takes to reduce the cardiovascular deaths double in numbers.
Results
The results reveal that the USA and China may lead in terms of raising its number of deaths caused by CVDs till 2027. However, doubling time model suggests that USA may require 2.3 years in reducing the cardiovascular deaths.
Conclusions
This study is significant for the policymakers and health practitioners to ensure the execution of CVD prevention measures to overcome the growing burden of CVD deaths.
Introduction
The upsurge of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection in early 2020 caused a disease pandemic known as COVID-19 [1, 2]. There is practically no country in the world which is not influenced by COVID-19 and the health services worldwide have never operated under this tremendous burden. Everything begun in Wuhan [3], China, but it has expanded exponentially all over the world. The core of the pandemic then moved to Europe and the US [4]. Studies also shown that patients with Cardiovascular Disease (CVD) are especially at great risk of COVID-19 mortality owing to their frailty and vulnerability [5, 6]. Patients with pre-existent CV risk factors and CVDs are among the most vulnerable with significantly greater risk of developing SARS-CoV-2 infection, acquiring CV complications associated with COVID-19, and having undesirable consequences [7].
Since the number of deaths has been increasing globally due to different reasons, CVD is one of the world’s most significant causes of mortality and morbidity. During the past decade, the number of deaths from CVD has increased by 12.5% globally [8, 9]. There are various reasons behind this progressive number of cardiovascular deaths. In 2016, the primarily cause of total global burden of CVD was ischemic heart disease (IHD) contributed to 49% of total burden of CVD, followed by stroke with 33% of total CVD burden. In comparison, other CVD causes account for a significantly lower percentage of the global disease burden [10].
CVDs have affected all the income level countries, especially low- and middle-income countries (LMIC) contribute the greatest portion to the overall CVD burden, specifically in terms of deaths at younger ages than in high-income countries, because of scarce human and financial resources [11,12,13]. Whereas, several of the largest LMIC had an increase in the overall burden of CVD; in decreasing pattern of percent burden increase, those included: India (15.4%), Bangladesh (27.4%), Indonesia (8.8%), China (6.6%), the Philippine (25.3%), and Mexico (19.7%) [14]. However, the CVD burden remains the most significant per capita in Eastern Europe and Central Asia. While, East Asia and South Asia are roots to the increased CVD burden, because of their growing and aging of the populations [15]. The 2016 Global Burden of Diseased Disease (GBD) report reveals that non-communicable diseases (NCDs) comprise 40% of the total age standardized global disease burden for women and about 50% of the global standardized men ‘s overall age burden. CVD alone accounted for 20% of women ‘s total burden and 24% of men ‘s total burden [16]. The frequency of steady or growing CVD Disability Adjusted Life-Year (DALY) epidemiological drivers vary across different countries. In countries such as Japan, a reduced CVD mortality rate has been offset by accelerated population aging. A slight rise of the CVD rate is associated with population ageing and limited resources in South Asian countries such as Pakistan, India, and Bangladesh [17].
Several epidemiological studies have forecast future trends in the occurrence of CVD and mortality rates for all age groups in various countries of the world [18,19,20], yet little is known about the absolute burden of deaths. To prepare for future cardiovascular care needs with certainty, the purpose of this study is to forecast the number of deaths caused by CVD from 2020 to 2027 of six higly effected countries which include Pakistan, India, China, Keyna, the USA and Sweden. We employed advanced mathematical modeling, namely Non-Homogenous Discrete Grey Model (NDGM) to predict the cardiovascular deaths of selected countries. The grey forecasting models, especially, the NDGM model, can be superior to other forecasting models in the context of small samples and poor information [21]. Hence, we have utilized NDGM model in the current paper to predict the future trends of CVD of top six countries globally. Further, a novel Synthetic Relative Growth Rate (RGR) and Synthetic Doubling Time (Dt) models employed to undertake a comparative analysis of CVD relative growth rate among six countries. Moreover, Mean Absolute Percentage Error (MAPE) % criterion was used to measure the accuracy of NDGM model. Hence, present research is a pioneer study to forecast relative growth and required time to reduce the number of deaths double in number caused by CVD among six countries. The study is principally significant for the policymakers to convey, empower and stimulate the execution of CVD prevention approaches to end this growing burden of CVD during the ongoing COVID-19 pandemic and time ahead.
The rest of paper follow as: Section 2 represent the research methodology. Whereas the result and discussion section are presented in section 3. Finally, conclusion, policy implications along with study limitations presented in last section is study.
Research methodology
This section provides steps involved in development of NDGM model. Additionally, synthetic RGR and synthetic Dt models have been discussed to analyze the growth and time of CVD deaths for selected countries. Finally, the performance evaluation of NDGM model through MAPE is also elaborated in this section.
Data source and study population
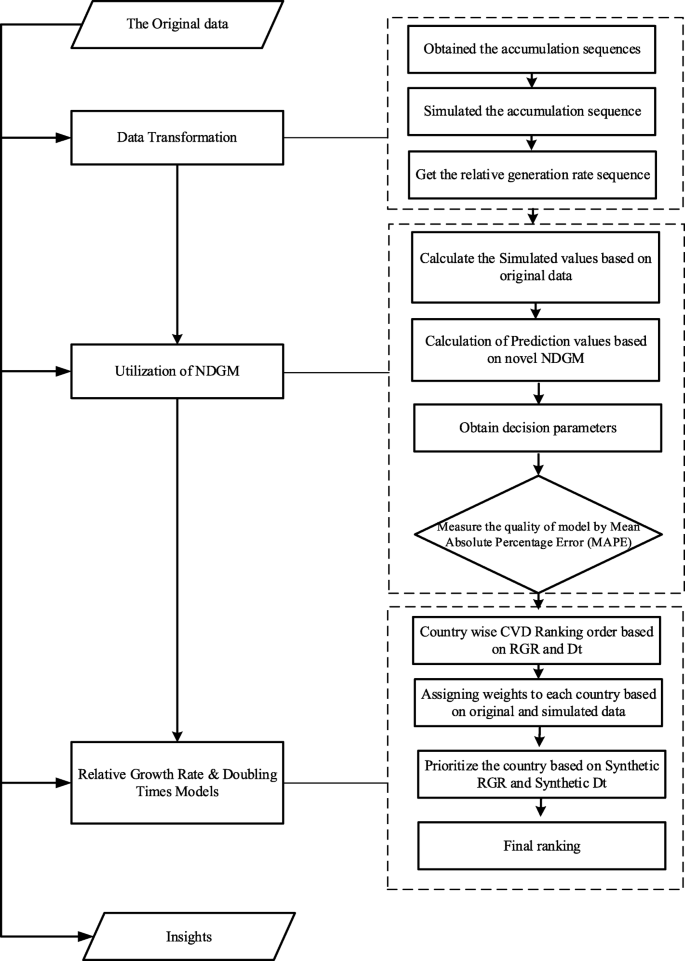
The CVD number of deaths data was abstracted from the official website of Our World in Data for the period 2005–2019. The top six countries which are Pakistan, India, China, Kenya, USA and Sweden with highly affected from cardiovascular deaths were selected, globally. The source of the data available at Our World in Data was the global burden of disease (GBD) collaborative network (2016), World Health Organization (WHO) and Institute for health metrics and evaluation (IHME) 2017. Grey system software (v8.0) has been used to forecast cardiovascular deaths for the period of 2020 to 2027 by NDGM. However, MATLAB and MS EXCEL were also used to solve NDGM. The current analysis and modeling methodology were employed for the first time in the study of forecasting CVD related deaths. The structure of forecasting the CVD deaths is operationalized in this study presented in Fig.1.
Grey forecasting model
In 1982 Deng Julong originally introduced the concept of a Grey Systems Theory (GST) as a scientific theory for predicting uncertain system, which involves limited and inadequate information. Ultimately, theoretical forecasts based on the grey framework surpassed the standards of statistical and mathematical methods [22]. Theory of grey systems has been applied successfully in several fields so far [23,24,25] and grey prediction theory is a significant branch of the theory of grey systems. There are five major types of grey prediction, such as time series forecasts, calamity forecasts, seasonal calamity forecasts, topological forecasts, and systemic forecasts. Till date, GS theory has introduced a variety of theories and techniques like grey mathematics, grey modeling, grey forecasting, grey clustering, grey decision making, grey programming, grey relational analysis, and grey control, which has been effectively implemented in various fields and has shown satisfactory results [26, 27]. The key benefit of grey theory is that it can manage both with limited and uncertain information with great precision. It functions as an analytical tool particularly in situations where data is inadequate.
Nonhomogeneous discrete grey model (NDGM)
In order to predict data, there are different types of grey models, we will analyze NDGM to predict future cardiovascular deaths. The NDGM system is designed on the basis of law of approximation non-homogenous exponential growth in accordance with assumptions of a sequence of real data [24] [28];. Xie et al. [25] recommended that the actual data sequence is a concurrence with a homogenous pattern like GM (1, 1). The accuracy level of NDGM model is considerably improved over other grey models so far as mean sequence value and value set of intervals [29]. NDGM model has been utilized in various fields, for example, in a study the electricity consumption of Turkey was predicted and analyzed the NDGM as best fit and more accurate prediction model over other grey forecasting models [30]. Whereas, Duan et al. forecast the crude oil consumption in China and investigated that NDGM showed superior performance [31].
x(0), represent the original data sequence and x(1) follows the accumulated data sequence in NDGM model so, we can write as follows:
Where, \( {\hat{x}}^{(1)} \) (L), is the forecasting value of x(1) along with parameters β 1, β 2, β 3 and β 4. So, we can write the above equation in matrix form as this: if L = 1, 2, and 3 …. n-1
The input data shows constant sequence in single case in order to satifsy NDGM parameters β1, β2, β3, and β4 by applying the following relation:
The following formula to be used to calculate β4 for minimizing the sum of square error:
For further knowledge about NDGM model, its parameter and properties, Liu et. al. (2010) is referred [25].
Performance evaluation approach of NDGM
We employed mean absolute percentage error (MAPE) to evaluate the accuracy of NDGM model. The formula to calculate MAPE % is as follows:
Where y(0)(k) represents the original sequence of data and \( {\hat{y}}^{(0)}(k) \) denotes the forecasting sequence data values.
Relative growth rate (RGR) and doubling time (Dt) analysis
To best of our knowledge, there is no model available to check the growth rate for cardiovascular deaths. In this manner, RGR model was used to analyze the relative growth of cardiovascular deaths for selected countries [32]. Two parameters (Dt and RGR) were employed in order to forecast the number of deaths caused by CVD of selected countries by utilizing NDGM model. The equation of RGR is given by,
Where L2 denotes the cumulative number of cardiovascular deaths in year t2 & L1 represent the cumulative number of cardiovascular deaths in year t1,as in our case, the equation can be reduced to
The Dt is the time required for publications to reduce the number of cardiovascular deaths for a given RGR is represented as:
In our case, it can be written as:
Synthetic RGR and synthetic doubling time model
In any case, if the RGR and Dt make an alternate pattern, when compared with that of actual data pattern create issue, in this regard synthetic Relative Growth Rate (RGRsyn) and Synthetic Doubling Time (Dsyn) models have been introduced [33]. The equation for Synthetic Relative Growth Rate (RGRsyn) model can be written as follows:
Whereas RGRoriginal denotes the Relative Growth Rate of original data and RGRforecast explains the Relative Growth Rate of predicted values. However, θ indicate relative weights coefficient and its value can be taken as 0.5 in general.
The Synthetic Doubling Time (Dsyn) model is presented as:
Here, Doriginal demonstrates the Doubling Time obtained from original data values, whereas RGRforecast indicate Relative Growth Rate based on forecasting data values.
Results
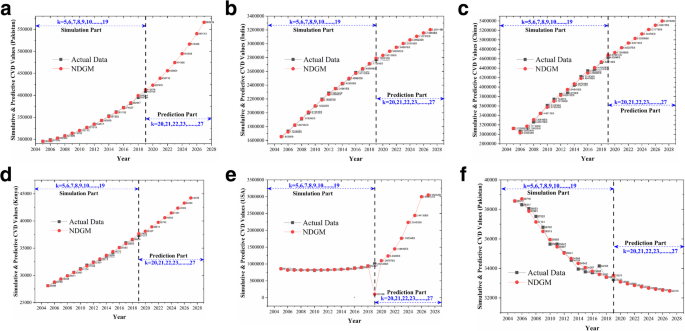
We employed NDGM to forecast the relative growth of cardiovascular deaths among six participated countries. The calculated simulated values for the data 2005–2019 are shown in Tables 1, 2, 3, 4, 5, and 6. Table 1 shows the forecasts results for Pakistan. The values obtained from MAPE % demonstrate the effectiveness level of 97.05% which shows NDGM as a best-fit grey model to forecast number of deaths caused by CVD. The simulated values based on NDGM showed an increasing trend for future. Figure 1 has been shown to better understand the comparison between actual data and the simulated NDGM data from 2005 to 2027 against the increasing deaths pattern for CVD in Pakistan.
With the turn of the century, CVDs became the leading cause of mortality in India. Table-2 represents the results from India with the MAPE accuracy level of 98.35%. The NDGM based simulated values also showed an inclined pattern in progressive number of cardiovascular deaths in future.
Table 3 represents the results for china. The forecast values based on NDGM simulated data showed an anticipated trend until 2027. The MAPE accuracy level turned out to be 96.88%. The NDGM model findings are found consistent with a range of other cardiovascular disease predictions in China, as the burden of CVD was increasing and primary and secondary prevention is likely to be core health policy priorities in the immediate future [34, 35].
Likewise, Tables 4, 5 and 6 represents the results for Kenya, USA and Sweden with MAPE accuracy level of 97.77, 96.8 and 97.74% respectively (Table 8). These findings are similar with some prior findings in which increasing trends have been reported [36]. According to a study in USA if projected trends in ischemic stroke mortality continue, increase in US stroke deaths will outpace overall population growth, with a doubling in deaths by the year 2032 [37]. For an easy and clear comparison of cardiovascular raising trends, Fig. 2a-f can be seen. All participated countries showed an increasing trend in raising their number of cardiovascular deaths, except for Sweden. A study has reported decline in mortality and incidence of cardiovascular related diseases since 1980s in Sweden. Changes in lifestyle have helped to break the increasing trend in CVD [38]. The outcomes reveal that the MAPE accuracy level for NDGM in case of India is found slightly higher than the rest of the five countries whereas Pakistan, Kenya and Sweden showed almost same MAPE accuracy level. The average MAPE accuracy level for NDGM showed a value of 97.44% (Table 8). The anticipated future trends in cardiovascular deaths for the participated countries compel to focus on the importance of increased investment in prevention and treatment of CVD.
a Simulative and Predictive values of NDGM for Pakistan. b Simulative and Predictive values of NDGM for India. c Simulative and Predictive values of NDGM for China. d Simulative and Predictive values of NDGM for Kenya. e Simulative and Predictive values of NDGM for USA. f Simulative and Predictive values of NDGM for Sweden
CV death growth and doubling time model based on NDGM
The relative growth rates and doubling time model have been employed to calculate the relative growth of cardiovascular deaths and an expected time to reduce the deaths in selected countries. Table 7 represents the ranking order of six countries for an estimated RGR and doubling time (Dt) as per original and simulated data. The RGR equation of original data showed a ranking order given below:
To calculate the required time for cardiovascular death reduction among six countries based on original data, the following sequence was observed as per doubling time (Dt) model:
The above-mentioned findings demonstrate that the relative growth of cardiovascular deaths in China as an upper middle-income country and USA as a high-income country rank higher followed by India, Pakistan, Kenya and Sweden based on original data. On the contrary, the doubling time model suggest that developed countries like USA and Sweden require an additional time and endeavors to reduce cardiovascular deaths double in number than in developing countries (India, Pakistan, China, Kenya). Therefore, the relative growth rate can be a source of competitive edge among developing and developed countries.
Likewise, we utilized NDGM-based simulated data to find out the status of deaths due to CVD for the period from 2020 to 2027. As indicated by RGR sequence, the following results was acquired:
Approximately same sequence was observed based on the simulated data. For the period 2020–2027, USA and China may endure progressively number of deaths due to CVD in terms of RGR i.e. (3.29%) and (2.75%) respectively followed-by Pakistan, Kenya, India and Sweden.
As per doubling time (Dt) model, the following pattern of results is obtained:
Our findings also revealed that USA and Sweden need relatively additional timespan to double reduce the number of cardiovascular deaths, followed by Kenya, India, Pakistan and China.
By using NDGM (based on actual and simulated data), we forecast the number of cardiovascular deaths for the period from 2020 to 2027.
Synthetic RGR and synthetic DTM for cardiovascular deaths
Presently a query arises here eventually as which country may endure maximum number of deaths by CVD in the long run. Therefore, to respond the query synthetic indices by original and forecasting values have been calculated.
By using synthetic indices, the sequence obtained for RGR is as follows:
As per synthetic doubling time model Dt, we obtained a sequence as follows:
Both sequences are found almost similar to the sequences obtained against the actual data thus the results are aligned with the actual data and the feasibility of the synthetic models has also been tested successfully.
Discussion
In spite of significant reductions in incidence and mortality, CVDs are still the greatest reason for death globally, both in terms of health and economic cost. We built up a forecasting framework to estimate the expected number of cardiovascular deaths in Pakistan, India, China, Kenya, the USA and Sweden by utilizing the most accurate methodology of the grey forecasting framework. Results depicted that grey prediction model was effectively applied to forecast the number of deaths caused by CVD for the period from 2020 to 2027. In addition, this study also suggests an expected time to reduce the number of deaths double in numbers using doubling time (Dt) formula. All six countries showed an increasing trend in forecasting number of deaths due to CVD for the period 2020–2027, except for Sweden. However, the results indicated that USA and China are more likely to suffer from cardiovascular deaths in future followed by Pakistan, Kenya, India and Sweden. Though China found prone to suffer maximum deaths in future, the doubling time (Dt) suggests less time expected to control and prevent from cardiovascular deaths double in number.
The results confirm that developed countries need relatively more time to reduce the deaths double in numbers whereas, developing countries require less time to do so. Whereas the USA and China may lead in terms of raising its cardiovascular mortality in future. While in case of lower middle-income countries, India and Pakistan are more likely to suffer from cardiovascular deaths in future followed by Kenya and Sweden. Figuratively speaking, a sword of Damocles hangs over the people of the USA and China, indeed most of the entire world, for the near future. Through CVD prevention and the implementation of workable approaches, we are foreseeing a future wherein the CVD epidemic is being tamed.
Statistics from various parts of the world show a large percentage of cerebrovascular and CV associated diseases in patients with COVID-19, which posed several questions about the higher sensitivity of patients with any of these comorbidities to the novel coronavirus, and also the function of CVD in progression and COVID-19 patient prognosis. Patients with Cardiovascular diseases should be monitored by their healthcare professionals with special preventive procedures for COVID-19 infection. The level of severity of both the primary respiratory syndrome and risk of adverse events is elevated in patients associated with COVID-19 and also with pre-existing cardiovascular diseases. Hospitals and health care networks must embrace a comprehensive approach to provide all patients with the best quality treatment, irrespective of their COVID-19 status. This is especially significant for the cardiology community, considering patients with prior symptoms of CVD and risk factors are potentially more likely to experience COVID-19 and encounter undesirable consequences. As the rate of infection rises, several cardiac patients may seek immediate treatment for either COVID-19 associated diseases or common cardiac complications. Most of these patients would need a cardiac intervention while at the same time getting SARS-CoV-2 infection.
COVID-19, triggered by SARS-CoV-2, is a worldwide pandemic emerging in real time. Cardiovascular and associated comorbidities are very common in COVID-19 patients and those are at greater risk of morbidity and mortality. COVID-19 raised an additional constraint on pre-existing CVDs. Findings from COVID-19 infection with a significant number of patients showed that fatality rate was of 10.5% for CVD among 72,314 COVID-19 cases [39]. Studies have revealed that there is a greater risk of mortality among patients hospitalized with COVID-19 due to CVD. Given the growing number of COVID-19 patients other than regular clinical presentations of illness, CVD in COVID-19 infected patients appear to be alarming [40, 41]. CVDs have played an important role in patient outcomes infected from the virus. Thus, careful review and monitoring of CVD in COVID-19 patients are required, from diagnosis to bedside.
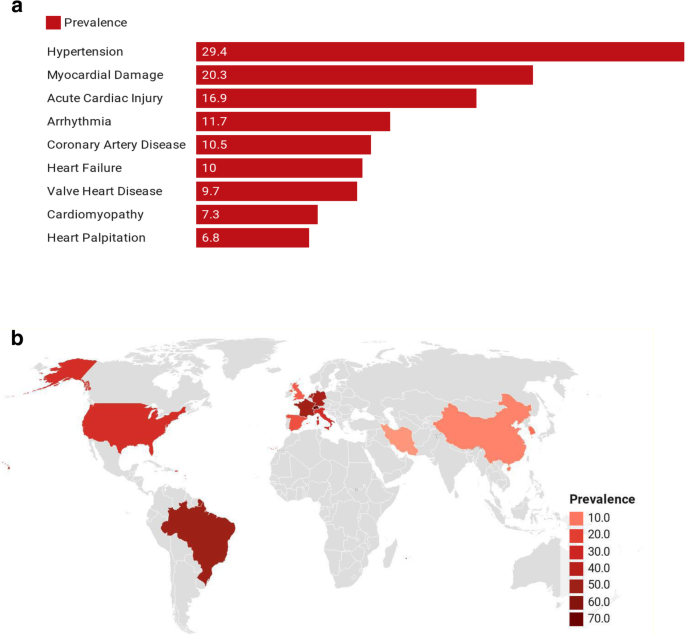
CV associated complications have been identified in prior respiratory infections with related etiology and their occurrence affects the severity of the illness, so even pneumonia related hospitalization is found related with long-term and short-term risk of CVD [42]. Infection from viruses lead to an imbalance in cardiac supply and demand, as well as an increase in systemic inflammation. Consequently, patients with pre-existing CVD are more likely to experience acute cardiac complications, and thrombosis, and lead to severe infections. An investigation from a meta-analysis analyzed pooled prevalence of CVD in COVID-19 infected patients in various countries. The following are the findings of the meta-analysis: the US (24%), Brazil (50%), Netherlands (44%), Germany (46%), Iran (4%), Italy (25%), China (8%), South Korea (11%), Spain (17%), Switzerland (71%), United Kingdome (15%), and France (48%) Fig. 3a. The prevalence of CV complications in infected patients was shown to be substantially correlated with ICU admissions and mortality in that meta-analysis Fig. 3b [44].
However, valid information to assess the exact burden of CVD is inadequate in many parts of the world, which compels the foundation of nationwide prevention and management policies. It is clear that while many advances have been introduced in our comprehension of worldwide CVD epidemiology, there is wide variation present in data, mainly in MICs and LICs such as Pakistan and India. In these regions, there is a requirement for significantly advanced frameworks for the supervision of risk factors and disease and for strategies that can diminish CVD’s morbidity and mortality at a low cost in ways that are practical and sustainable. The former can be achieved with large but simple health surveys that gather reliable data on health behaviors, CVD associated risk factors, incidence, and mortality, and access to health care in every region of the world.
Though these predictions are sober, they do not need to become true, as CVD is potentially preventable. Improving risk factors at population level in the past obviously had a decisive effect on the reduction in death rates for CVD worldwide. Several studies have shown that there is a considerable decrease in CVD mortality rates among individuals with favorable levels of significant CVD risks [45] [8, 46]. Likewise, people who practice a healthy lifestyle face a comparatively lower risk of suffering from cardiovascular related diseases. A greater emphasis on prevention may therefore alter these anticipated trends in the future and eventually may overcome the growing pandemic of COVID-19.
Limitations
The present study has several limitations. The data from Our World in Data, however comprehensive and easily accessible to almost all countries and regions, is based on regularly available data from those countries and regions. Variations may occur in the robustness of the data selection and processing and reliability of the cause of the death. Secondly, these predictions are made for developed and developing countries data together, and their generalizability to other countries should be considered with caution. It should be acknowledged that there are many differences between developed and developing countries when comparing health-care systems and how diseases are dealt. We believe that this has kept our analysis conservative. Another limitation of the study is the application of single grey prediction model which is NDGM. The further research can be carried out by employing other grey prediction models and should consider the other regions of the world for more insight information.
Conclusion
In conclusion, CVD plays a key role in disease burden and mortality in COVID-19 patients. Since CVD complications in COVID-19 patients could be fatal, they must be carefully monitored and managed in the case of an acute illness. It is yet not clear whether the prevalence of cardiovascular comorbidities poses independent risk or if this is affected by other factors such as age etc. The results from the forecasting model against all selected countries showed an increasing trend in terms of raising its number of deaths due to CVD till 2027, except for Sweden. However, the growth rate for the USA (RGR: 2.71%) and China (RGR: 2.55%) was found relatively higher than the rest of the three countries. The findings also revealed that USA (2.3 years) and Sweden (2.2 years) may require relatively additional timespan to double reduce the number of cardiovascular deaths when compared with China (2.1 years). The findings of this study can aid policymakers, doctors, and front-line healthcare workers in making evidence-based decisions and reducing the mortality and morbidity associated with this 21st-century pandemic.
Availability of data and materials
The data used in the current study is available publicly at www.ourworldindata.com.
Change history
12 July 2021
A Correction to this paper has been published: https://0-doi-org.brum.beds.ac.uk/10.1186/s12889-021-11450-z
Abbreviations
- CVD:
-
Cardiovascular disease
- NDGM:
-
Non-homogeneous discrete grey model
- EGM:
-
Even Grey Model
- DGM:
-
Discrete Grey Model
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- RGR:
-
Relative Growth Rate
- Dt :
-
Doubling Time
- GST:
-
Grey Systems Theory
- IHD:
-
Ischemic Heart Disease
- LMICs:
-
Low- and middle-income Countries
- GBD:
-
Global Burden of Disease
- NCDs:
-
Non-communicable diseases
- DALY:
-
Disability adjusted life-years
- MAPE:
-
Mean Absolute Percentage Error
- WHO:
-
World Health Organization
- IHME:
-
Institute of health metrics and evaluation
References
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–62. https://0-doi-org.brum.beds.ac.uk/10.1016/S0140-6736(20)30566-3.
Siddiqi HK, Neilan TG. COVID-19, Immuno-oncology and cardiovascular disease: viewpoint from the intersection. J Cardiovasc Transl Res. 2020;13(3):347–8. https://0-doi-org.brum.beds.ac.uk/10.1007/s12265-020-10013-8.
Liu Z, Magal P, Seydi O, Webb G. Understanding unreported cases in the COVID-19 epidemic outbreak in Wuhan, China, and the importance of major public health interventions. Biology. 2020;9:50.
Tadic M, Cuspidi C, Mancia G, Dell’Oro R, Grassi G. COVID-19, hypertension and cardiovascular diseases: Should we change the therapy? Pharmacol Res. 2020;13:104906.
Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Syndr Clin Res Rev. 2020;14(3):247–50. https://0-doi-org.brum.beds.ac.uk/10.1016/j.dsx.2020.03.013.
Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, et al. COVID-19 and cardiovascular disease. Circulation. 2020;141(20):1648–55. https://0-doi-org.brum.beds.ac.uk/10.1161/CIRCULATIONAHA.120.046941.
Ganatra S, Dani SS, Shah S, Asnani A, Neilan TG, Lenihan D, et al. Management of cardiovascular disease during coronavirus disease (COVID-19) pandemic. Trends Cardiovasc Med. 2020;30(6):315–25. https://0-doi-org.brum.beds.ac.uk/10.1016/j.tcm.2020.05.004.
Joseph P, Leong D, McKee M, Anand SS, Schwalm JD, Teo K, et al. Reducing the global burden of cardiovascular disease, part 1: the epidemiology and risk factors. Circ Res. 2017;121(6):677–94. https://0-doi-org.brum.beds.ac.uk/10.1161/CIRCRESAHA.117.308903.
Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol. 2017;70:1–25.
Watkins DA, Beaton AZ, Carapetis JR, Karthikeyan G, Mayosi BM, Wyber R, et al. Rheumatic heart disease worldwide: jacc scientific expert panel. J Am College Cardiol. 2018;72:1397–416.
Bowry ADK, Lewey J, Dugani SB, Choudhry NK. The burden of cardiovascular disease in low-and middle-income countries: epidemiology and management. Can J Cardiol. 2015;31(9):1151–9. https://0-doi-org.brum.beds.ac.uk/10.1016/j.cjca.2015.06.028.
Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P. The economic burden of cardiovascular disease and hypertension in low-and middle-income countries: a systematic review. BMC Public Health. 2018;18(1):975. https://0-doi-org.brum.beds.ac.uk/10.1186/s12889-018-5806-x.
Rehman S, Li X, Wang C, Ikram M, Rehman E, Liu M. Quality of care for patients with acute myocardial infarction (AMI) in Pakistan: a retrospective study. Int J Environ Res Public Health. 2019;16(20):3890. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16203890.
Yusuf S, Rangarajan S, Teo K, Islam S, Li W, Liu L, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med. 2014;371(9):818–27. https://0-doi-org.brum.beds.ac.uk/10.1056/NEJMoa1311890.
Ohira T, Iso H. Cardiovascular disease epidemiology in Asia. Circ J. 2013;2013:CJ-13.
Benziger CP, Roth GA, Moran AE. The global burden of disease study and the preventable burden of NCD. Glob Heart. 2016;11(4):393–7. https://0-doi-org.brum.beds.ac.uk/10.1016/j.gheart.2016.10.024.
Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372:1333–41.
Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123(8):933–44. https://0-doi-org.brum.beds.ac.uk/10.1161/CIR.0b013e31820a55f5.
Chernova IV, Sumin SA, Bobyr MV, Seregin SP. Forecasting and diagnosing cardiovascular disease based on inverse fuzzy models. Biomed Eng. 2016;49:263–7.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2018;137(12):e67–492. https://0-doi-org.brum.beds.ac.uk/10.1161/CIR.0000000000000558.
Ikram M, Sroufe R, Zhang Q, Ferasso M. Assessment and prediction of environmental sustainability: novel grey models comparative analysis of China vs. the USA. Environ Sci Pollut Res. 2021;28(14):17891–912. https://0-doi-org.brum.beds.ac.uk/10.1007/s11356-020-11418-3.
Chiang JS, Wu PL, Chiang SD, Chang TJ, Chang ST, Wen KL. Introduction to Grey system theory. J Grey Syst. 1998;1:1–24.
Rehman E, Ikram M, Feng MT, Rehman S. Sectoral-based CO2 emissions of Pakistan: a novel Grey relation analysis (GRA) approach. Environ Sci Pollut Res. 2020;27(23):29118–29. https://0-doi-org.brum.beds.ac.uk/10.1007/s11356-020-09237-7.
Javed SA, Liu S. Predicting the research output/growth of selected countries: application of even GM (1, 1) and NDGM models. Scientometrics. 2018;115(1):395–413. https://0-doi-org.brum.beds.ac.uk/10.1007/s11192-017-2586-5.
Xie N-M, Liu S-F, Yang Y-J, Yuan C-Q. On novel grey forecasting model based on non-homogeneous index sequence. Appl Math Model. 2013;37(7):5059–68. https://0-doi-org.brum.beds.ac.uk/10.1016/j.apm.2012.10.037.
Wu L-F, Liu S-F, Cui W, Liu D-L, Yao T-X. Non-homogenous discrete grey model with fractional-order accumulation. Neural Comput Appl. 2014;25(5):1215–21. https://0-doi-org.brum.beds.ac.uk/10.1007/s00521-014-1605-1.
Ikram M, Zhang Q, Sroufe R. Developing integrated management systems using an AHP-fuzzy VIKOR approach. Bus Strateg Environ. 2020;29(6):2265–83. https://0-doi-org.brum.beds.ac.uk/10.1002/bse.2501.
Liu S, Forrest JYL. Grey systems: theory and applications: Springer; 2010. https://0-doi-org.brum.beds.ac.uk/10.1007/978-3-642-13938-3.
Ikram M, Mahmoudi A, Shah SZA, Mohsin M. Forecasting number of ISO 14001 certifications of selected countries: application of even GM (1,1), DGM, and NDGM models. Environ Sci Pollut Res. 2019;26(12):12505–21. https://0-doi-org.brum.beds.ac.uk/10.1007/s11356-019-04534-2.
Kusakci AO, Ayvaz B. Electrical energy consumption forecasting for Turkey using grey forecasting technics with rolling mechanism. In: Conference Proceedings of 2015 2nd international conference on knowledge-based engineering and innovation: KBEI 2015. Tehran: Iran University of Science and Technology; 2016.
Duan H, Lei GR, Shao K. Forecasting crude oil consumption in China using a grey prediction model with an optimal fractional-order accumulating operator. Complexity. 2018;2018:1–12. https://0-doi-org.brum.beds.ac.uk/10.1155/2018/3869619.
Bajwa RS, Yaldram K, Rafique S. A scientometric assessment of research output in nanoscience and nanotechnology: Pakistan perspective. Scientometrics. 2013;94(1):333–42. https://0-doi-org.brum.beds.ac.uk/10.1007/s11192-012-0699-4.
Liu S, Yang Y, Forrest J. Grey data analysis. Singapore: Springer; 2017.
Shen C, Ge J. Epidemic of cardiovascular disease in China: current perspective and prospects for the future. Circulation. 2018;138(4):342–4. https://0-doi-org.brum.beds.ac.uk/10.1161/CIRCULATIONAHA.118.033484.
Stevens W, Peneva D, Li JZ, Liu LZ, Liu G, Gao R, et al. Estimating the future burden of cardiovascular disease and the value of lipid and blood pressure control therapies in China. BMC Health Serv Res. 2016;16:1–10.
Pearson-Stuttard J, Guzman-Castillo M, Penalvo JL, Rehm CD, Afshin A, Danaei G, et al. Modeling future cardiovascular disease mortality in the United States: national trends and racial and ethnic disparities. Circulation. 2016;133(10):967–78. https://0-doi-org.brum.beds.ac.uk/10.1161/CIRCULATIONAHA.115.019904.
Elkins JS, Johnston SC. Thirty-year projections for deaths from ischemic stroke in the United States. Stroke. 2003;34(9):2109–12. https://0-doi-org.brum.beds.ac.uk/10.1161/01.STR.0000085829.60324.DE.
Bengtsson T, Keilman N. Old and new perspectives on mortality forecasting. Cham: Springer Nature; 2019.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–42. https://0-doi-org.brum.beds.ac.uk/10.1001/jama.2020.2648.
Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811–8. https://0-doi-org.brum.beds.ac.uk/10.1001/jamacardio.2020.1017.
Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential effects of coronaviruses on the cardiovascular system. JAMA Cardiol. 2020;5(7):831–40. https://0-doi-org.brum.beds.ac.uk/10.1001/jamacardio.2020.1286.
Violi F, Cangemi R, Calvieri C. Hospitalization for pneumonia and risk of cardiovascular disease. JAMA. 2015;313(17):1753. https://0-doi-org.brum.beds.ac.uk/10.1001/jama.2015.3130.
Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116(10):1666–87. https://0-doi-org.brum.beds.ac.uk/10.1093/cvr/cvaa106.
Hessami A, Shamshirian A, Heydari K, Pourali F, Alizadeh-Navaei R, Moosazadeh M, et al. Cardiovascular diseases burden in COVID-19: Systematic review and meta-analysis: medRxiv; 2020. https://0-doi-org.brum.beds.ac.uk/10.1016/j.ajem.2020.10.022.
Barber RM, Fullman N, Sorensen RJD, Bollyky T, McKee M, Nolte E, et al. Healthcare access and quality index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the global burden of disease study 2015. Lancet. 2017;390(10091):231–66. https://0-doi-org.brum.beds.ac.uk/10.1016/S0140-6736(17)30818-8.
Fuster V, Kelly BB, Vedanthan R. Promoting global cardiovascular health: moving forward. Circulation. 2011;123(15):1671–8. https://0-doi-org.brum.beds.ac.uk/10.1161/CIRCULATIONAHA.110.009522.
Acknowledgments
Not applicable.
Funding
This work is supported by the Union Program of Science and Health of Hunan Province, China (2019JJ80011). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
SR wrote the first draft of the article and conceptualized the overall study. SR and MI are involved in the data analysis. SR, ER and MI wrote the final manuscript. ZJL is responsible for project administration and supervision of the overall manuscript. All authors contributed to a second and third iteration of the manuscript, and everyone read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study used secondary data and did not involve human subjects directly, informed consent was not obtained from the patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised as it erroneously contained red text in the equations under the section Relative growth rate (RGR) and doubling time (Dt) analysis.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rehman, S., Rehman, E., Ikram, M. et al. Cardiovascular disease (CVD): assessment, prediction and policy implications. BMC Public Health 21, 1299 (2021). https://0-doi-org.brum.beds.ac.uk/10.1186/s12889-021-11334-2
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s12889-021-11334-2